Gymnastics is an extremely intense sport both emotionally and physically. The physical demands of this sport unfortunately leave gymnasts susceptible to almost any injury under the sun. Low back [lumbar] pain, specifically, is one of the many ailments common amongst gymnasts due to the sport’s repetitive nature. There are a number of diagnoses that may explain this low back pain experienced by so many gymnasts, but one of the most common diagnoses that may be relieved by physical therapy is Spondylosis or even Spondylothesis.
Diagnosis in Low Back Pain:
- Spondylosis is the degeneration of the spine due to overuse
- This unilateral or bilateral overuse involves the pars interarticularis of the posterior vertebral arch. This pars interarticularis defect, also referred to as a stress fracture, consists of fibrous tissue. 85-95% of defects occur in the lower lumbar region at L5, with L4 being the next most common vertebra.
- Lumbar instability may progress to spondylosis or even spondylothesis
- Spondylolisthesis is a progression of spondylolysis leading to forward displacement of one vertebral body in relation to the one below it, usually secondary to a bilateral pars defect. This displacement is progressive, especially during rapid growth spurts of early adolescence. It is most common at L5-S1.
Common Symptoms of Low Back Pain:
- Gradual onset of pain, progressively worsens
- Pain is a dull ache and worsens with activity
- Occasional sharp pain with certain activities or changing positions
- Pain with prolonged positions such as sitting or standing
- Pain restricts activities of daily living or sports performance
- May feel unstable or have a catching pain through motions not at end range
- Rest usually relieves symptoms
- Possible history of local trauma or a previous injury, but usually not from a specific incident
How Spondylosis occurs:
- Spondylosis occurs over time with a higher incidence in the young athletic population (gymnasts, football players, divers, wrestlers, weight lifters)
- It is commonly from excessive or repeated hyperextension activities which are extremely common in gymnastics, along with generalized laxity and lumbar hypermobility
- Weak core stabilizers, especially the transverse abdominis can also contribute to back pain. If the core is not stabilized with movement, the spine becomes the victim of excess motion and increased loading.
Differential Diagnoses:
- Spondylolisthesis
- Sprain/ Strain Injuries
- Disc Pathology
- Facet Joint Pathology
- SIJ Dysfunction
- Stress Fracture
Pertinent Tests/Diagnostic Imaging:
- Referral to MD for further imaging and evaluation
- Spondylolysis defect is known as the “Scottie Dog” appearance on X-rays
- If it has progressed to Spondylolisthesis, the severity will be graded on a I-IV scale depending on the amount of forward displacement of the vertebra
- Clinical Tests in PT
- + Prone Instability Test
- + Gower Sign
- + Reverse Spinal Rhythm deficits
- Clinical Prediction Rule for Stabilization Protocol: aberrant motion
- Observation, excessive flexibility in a straight leg raise (hamstring flexibility),
- + Prone Instability Test
Risk Factors of Low back pain:
- History of low back pain
- History of traumatic hyperextension
- Generalized hypermobility or diagnosis of a hypermobility disorder such as Ehlers-Danlos Syndrome
When To Seek Medical Attention:
- Persistent pain that does not improve with rest over time
- Palpable step off along the back (if the vertebra has slipped forward, an indent may be felt along the lower spine)
- Numbness or tingling sensation in the lower extremities (if the vertebra has slipped forward, it may be pressing on a nerve root and could cause sensation deficits)
Principles of Treatment:
- Course of anti-inflammatory medication may assist with pain relief and inflammation
- Osseous healing is not absolutely necessary for excellent clinical outcome
- Limit any activities that increase pain- modify practice/ training program, extension typically avoided
- Find rest and relief postures when sustaining positions that increase pain
- Spinal brace may be necessary if imaging suggests Spondylolisthesis
– Prevent motion at that spinal segment to allow the bone to heal
– Possible 3 months in brace with no PT, followed by PT with progressive return to sport - Focus PT on gluteus and core strengthening
– Strengthening, stabilization, and motor control is usually the focus of treatment - Safe extension activities- limit hyperextension in practice
- Safe return to gymnastics and proper loading patterns
– Movement analysis to address contributing factors
– Address movement deficits to prevent this from reoccurring
- Maintenance of strong supportive trunk muscles is very important, as well as sport specific training with a neutral spine, postural education, and sensorimotor control
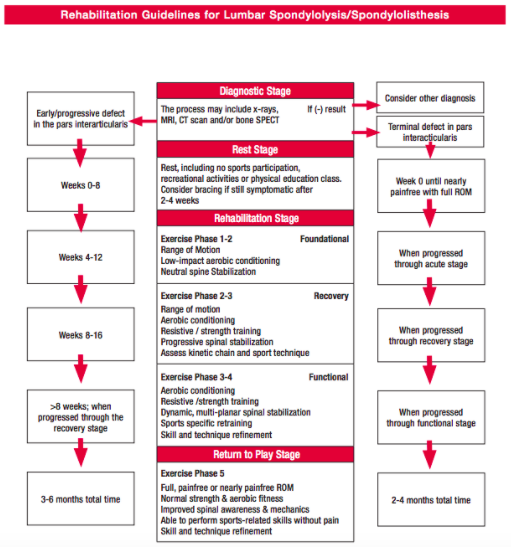
- Do not progress to new levels of rehab unless there is successful completion of the previous level without provocation of pain and normalized active range of motion
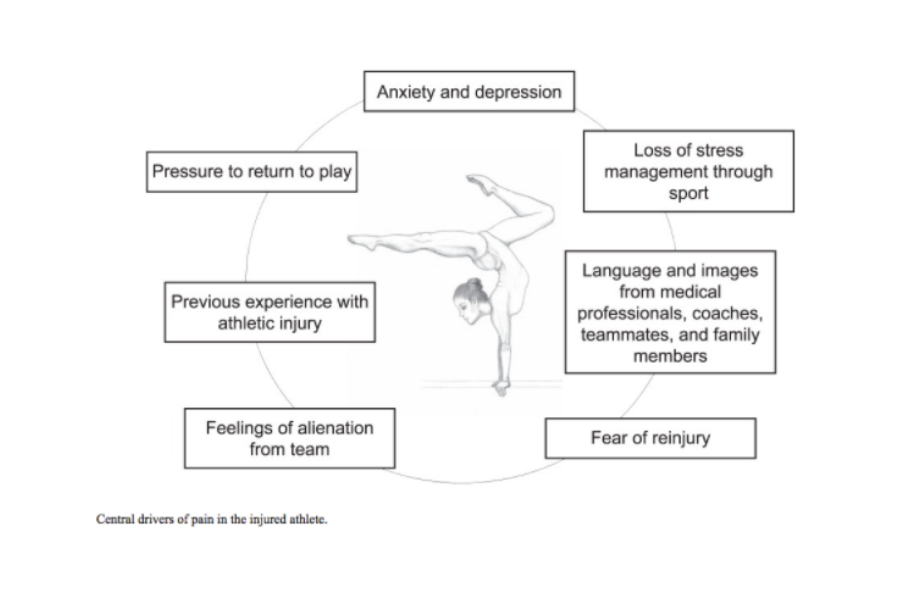
- It is also very important to address any psychosocial components that could be contributing to the gymnast’s pain. Young gymnasts often train at a high intensity from a very young age and are under a lot of pressure from coaches and teammates
Goals of Treatment to Low Back pain:
- Decrease pain
- Normalize tissue palpation and length
- Improve strength of individual muscles as well as overall functional strength
- Postural education and correction
- Improve dynamic stabilization
Return to Sport:
- Total rehabilitation time for return to sport is between 2-6 months
- Phase 1: Rest and Protect
- Phase 2: Static Stabilization
- Phase 3: Dynamic Trunk Stabilization and Coordination
- Phase 4: Athletic Enhancement and Gradual Return
- Phase 5: Independent Exercise Program and Re-Injury Prevention Program
- Return to gymnastics requires:
– Pain free ROM
– Improved functional strength
– Proper spinal awareness and body mechanics
– Technique refinement to ensure proper body mechanics when performing skills repetitively or when fatigued
PT Role and How to Prevent Spondylosis:
- Improve core and lumbar stabilization
- Postural education
- Education on training modifications
- Education on proper technique and body mechanics
- Screen for psychosocial risk factors
References:
– Cavalier, R., M. J. Herman, E. V. Cheung and P. D. Pizzutillo (2006). “Spondylolysis and spondylolisthesis in children and adolescents”
– Dankaerts, W., & O’Sullivan, P. (2011). The validity of O’Sullivan’s classification system (CS) for a sub-group of NS-CLBP with motor control impairment (MCI): overview of a series of studies and review of the literature. Manual therapy, 16(1), 9–14. doi:10.1016/j.math.2010.10.006
– Jackson DW, Wiltse LL, Cirincoine RJ. Spondylolysis in the female gymnast. Clinical orthopaedics and related research. 1976(117):68-73.
– Hoffman, S. L., Johnson, M. B., Zou, D., Harris-Hayes, M., & Van Dillen, L. R. (2011). Effect of classification-specific treatment on lumbopelvic motion during hip rotation in people with low back pain. Manual therapy, 16(4), 344–350. doi:10.1016/j.math.2010.12.007
– McNeely, M. L., G. Torrance and D. J. Magee (2003). “A systematic review of physiotherapy for spondylolysis and spondylolisthesis.” Man Ther 8(2): 80-91.
– Newell, R. L. (1995). “Spondylolysis. An historical review.” Spine (Phila Pa 1976) 20(17): 1950-1956
– Winslow JJ, Jackson M, Getzin A, Costello M. Rehabilitation of a Young Athlete With Extension-Based Low Back Pain Addressing Motor-Control Impairments and Central Sensitization. Journal of athletic training. 2018;53(2):168-173.